This is the last in a three-part series covering some of the ongoing problems in our current health care system.
Previous posts discussed the dramatic rise in deductibles and pharmaceutical price gouging. Today's focus is on another egregious practice of the health insurance industry: increased restrictions on patient choice of doctor and hospital.
Tightening the Reins on Patient Choice
Health insurance companies are dropping PPO plans like hot potatoes. PPO (preferred provider organization) plans allow patients to choose providers outside the plan's preferred network, while HMO plans restrict patients to only a limited network. Why are insurance companies doing this?
"It's probably because insurers have less control over costs with PPO plans because they (customers) can pick the doctors they want," explained Lisa Reid, director of life and health at the NM Office of the Superintendent of Insurance. (Albuquerque Journal, Sept. 15, 2015)
A Santa Fe New Mexican article expands on this:
"More than ever, the writing is on the wall. It's going to be harder for insurers of any size to keep offering PPOs in the exchange and individual markets," writes blogger Bill Melville, a senior analyst on health care exchanges with Decisions Resources Group in Nashville, Tenn. "The pathway to exchange profitability is narrow, and the statewide PPO networks are not."
Increasing restrictions regarding choice of provider include hospitals as well as physicians. For example, Blue Cross Blue Shield does not have a contract with Presbyterian's Albuquerque hospitals, which impacts Albuquerque-area residents. And it was recently announced that Santa Fe-area seniors covered by the Presbyterian Medicare Advantage Program (approximately 2,000 people) will not be able to use Christus St. Vincent Regional Medical Center, which is the only hospital in Santa Fe.
In the New Mexican article cited above, the president of Blue Cross Blue Shield of New Mexico asserts that in general, the company's PPO plans "are 10 percent to 20 percent more expensive than other types of coverage."
But that's just the insurance company's bottom-line perspective. It is important to note that the consumer is actually opting to pay extra for the right to select a provider or hospital that is not tied to his or her insurance company's network. These PPO policies require consumers to pay higher premiums, and patients may also end up with extremely large cost-sharing responsibilities in the form of deductibles, co-pays, and co-insurance.
There is no free ride here. So, while insurance companies are concerned about their "out of pocket" costs, consumers are definitely playing a big role in covering those expenses.
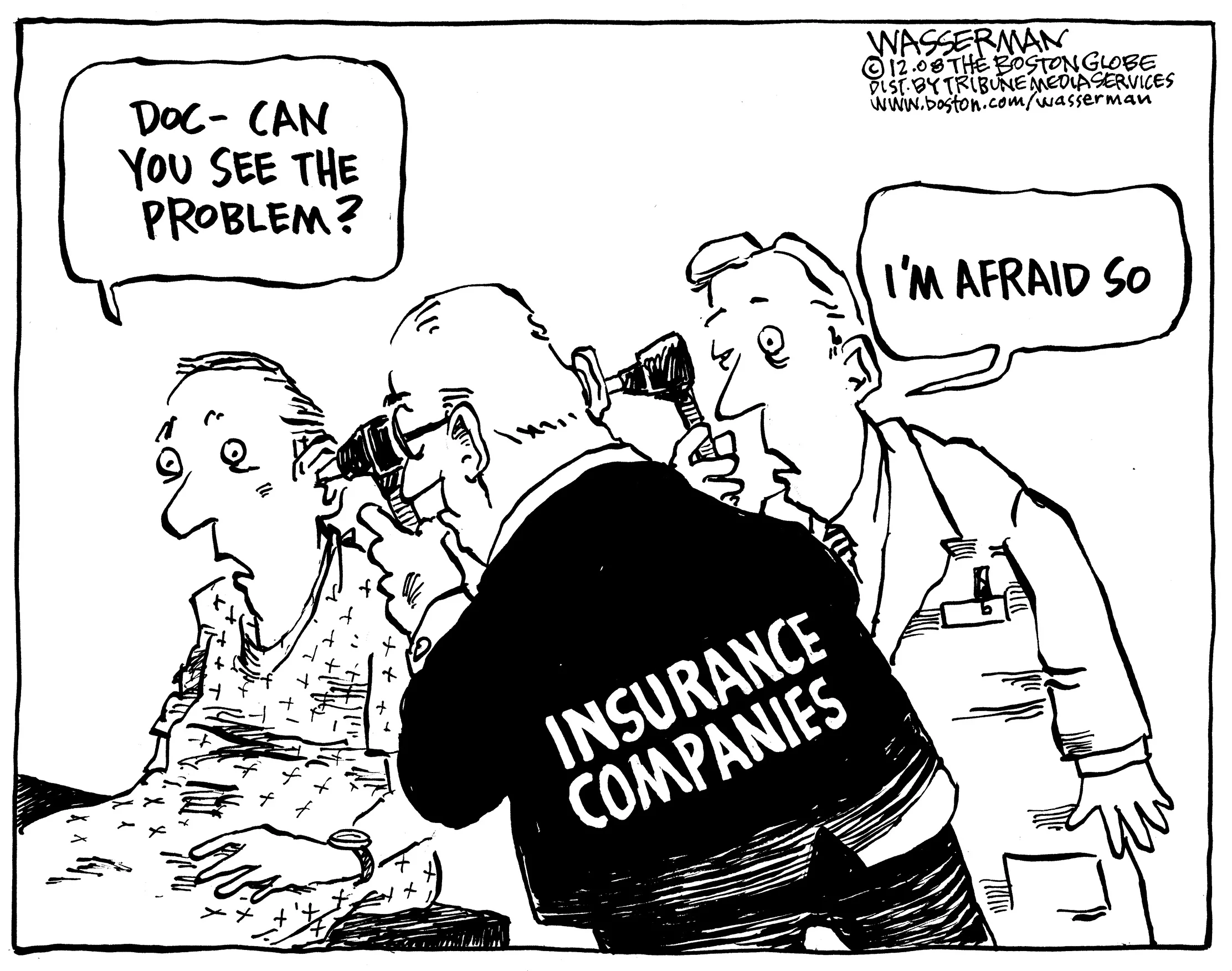
We are extremely thankful to Dan Wasserman for allowing us to reproduce another of his wonderful cartoons!
And, if that isn't enough to get you up in arms, even using an in-network facility doesn't guarantee access to in-network providers.
Patients may be charged thousands of dollars for the services provided at an in-network hospital because the anesthesiologist, surgeon, or other specialist at the hospital was not under contract with their insurance company.
One of the problems that arises with restrictive networks is that it's difficult to know exactly who is in them. And if your provider isn't in-network, your non-PPO insurance plan may not pay your bill. Unfortunately, choosing an in-network hospital does not mean that all costs are covered.
Consumers Union (the publisher of Consumer Reports) has initiated a national campaign to pass laws that will address the unexpected medical bills that too often are confronting patients with restricted networks. The impetus for the End Surprise Medical Bills campaign is clear:
"Simply put, loopholes mean there is no guarantee that when you go to an 'in-network' hospital or medical facility, you'll actually pay in-network prices. Picking a hospital on your insurance may still leave you with a big surprise if the anesthesiologist in the operating room isn't covered on your plan."
The Health Security Alternative
Under the New Mexico Health Security Plan, there will be no more networks. Consumers will be able to see any health care provider they want (as long as that provider has the availability, of course). The Plan, like any insurance carrier, can negotiate with providers across state lines so New Mexicans who use medical practitioners and facilities in neighboring states can continue to do so. In addition, Plan members will have access to specialists and specialty centers across the country.
The Health Security Plan also forbids balance billing. Balance billing is when you pay whatever balance is left on a bill after the insurance company has paid the agreed-upon negotiated rate.
How will this work from the provider side? The Health Security Plan will negotiate reimbursement rates with medical providers (with mandatory mediation if there is disagreement). Health care providers will also have a seat at the table: the governing commission for the Health Security Plan has 5 positions for health professionals (along with 10 for consumers and business owners).